Learn About CTCL Skin Symptoms

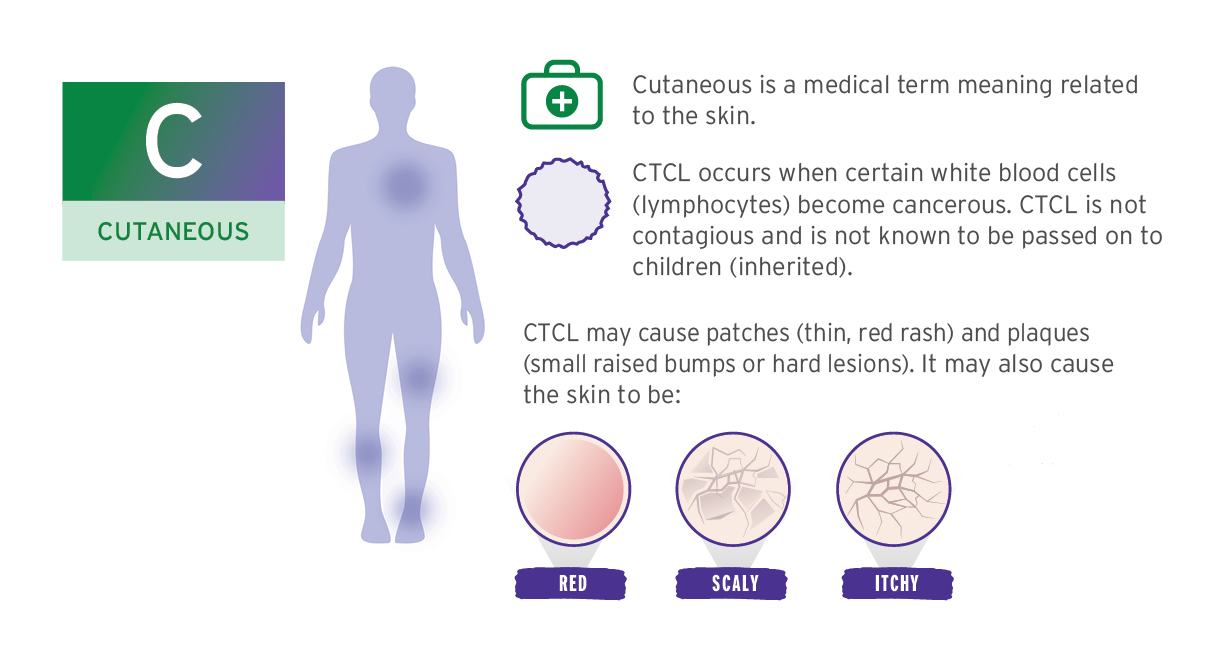
Cutaneous T-Cell Lymphoma (CTCL) is known for the red, scaly, itchy, skin symptoms and rash it may cause. CTCL skin symptoms can help doctors diagnose CTCL but they can also be confused with other diseases.
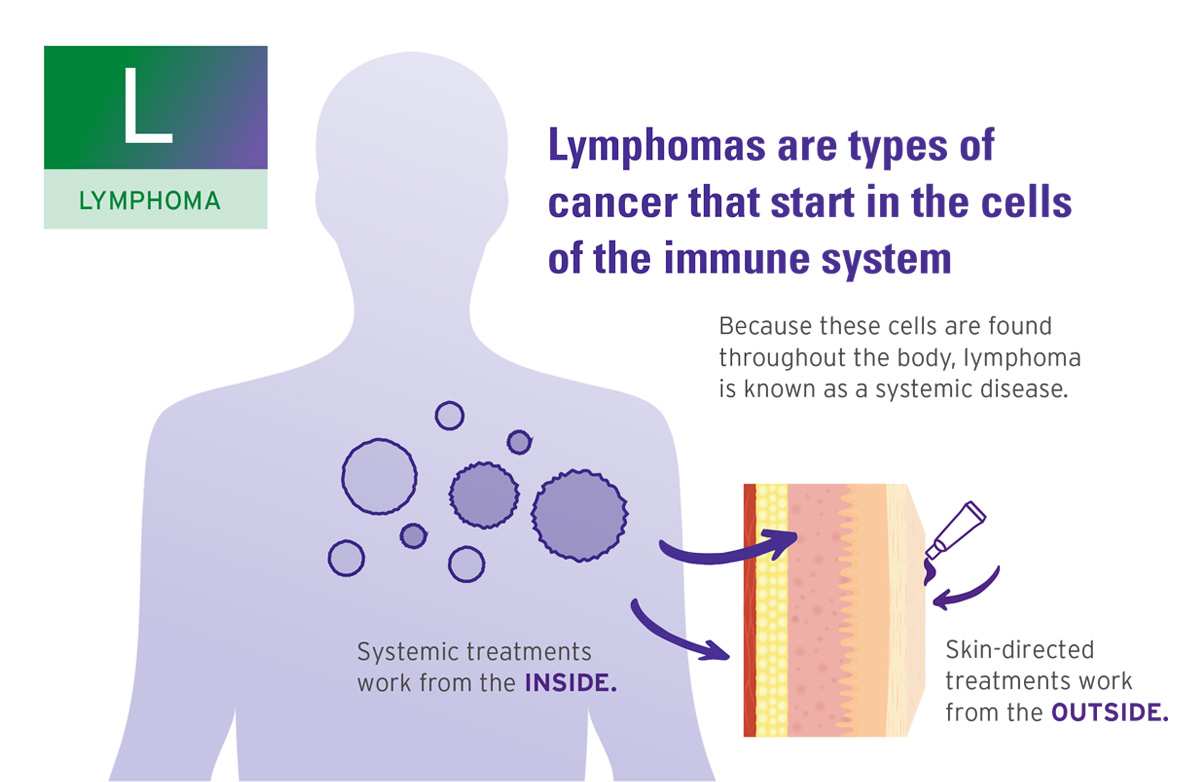
CTCL is a type of non-Hodgkin's lymphoma (a type of cancer). It is caused by cells that change in the blood and travel to the skin. CTCL is known as a systemic disease because these cells are found throughout the body.
Doctors diagnose CTCL based on signs, symptoms, and the results of blood and skin tests. They assign a stage to describe how advanced the disease is. CTCL staging also helps the healthcare team to find the right treatment to manage the skin symptoms of CTCL.
There are 2 main types of CTCL skin symptoms:
MYCOSIS FUNGOIDES (MF)
(my-KOH-sis fun-GOID-ees)
- The most common type of CTCL
- Tends to happen slowly over years
SÉZARY SYNDROME (SS)
(SEY-zhair-ee SIN-drohmm)
- A less common type of CTCL
- Happens faster
- Cancer cells are found in the blood and the skin
Treating the skin symptoms of CTCL
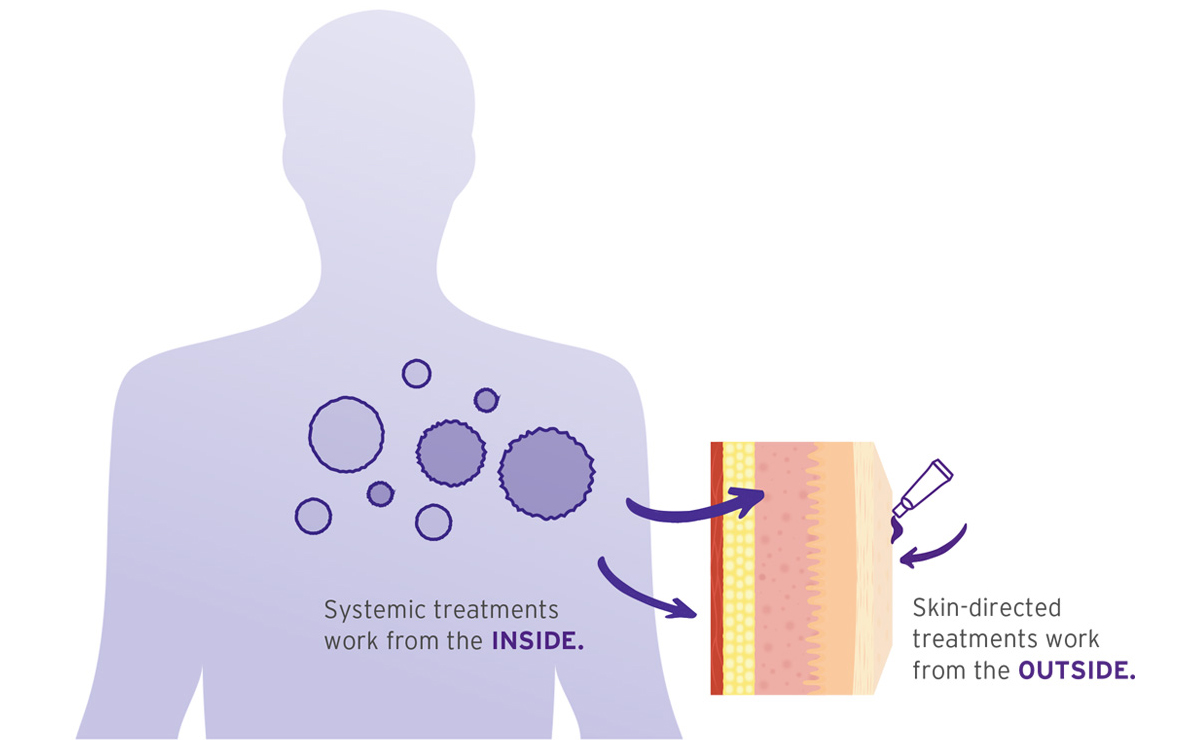
There are two main types of treatment for the skin symptoms of CTCL:
Skin-directed treatments
target skin lesions
- Ultraviolet (UV) light
- Steroids
- Local radiation
- Chemotherapy (put on the skin)
- Retinoids (put on the skin)
Systemic treatments
work throughout the body
- Photopheresis
- Retinoids (taken by mouth)
- Interferon
- Chemotherapy (taken by mouth or through an IV)
Talk with your healthcare team about your CTCL skin symptoms and treatments that may help to control them.
Get answers to some common questions about CTCL skin symptoms
Remember that your healthcare team is always the best source of information about your diagnosis and treating your skin symptoms.
What is Cutaneous T-Cell Lymphoma (CTCL)?
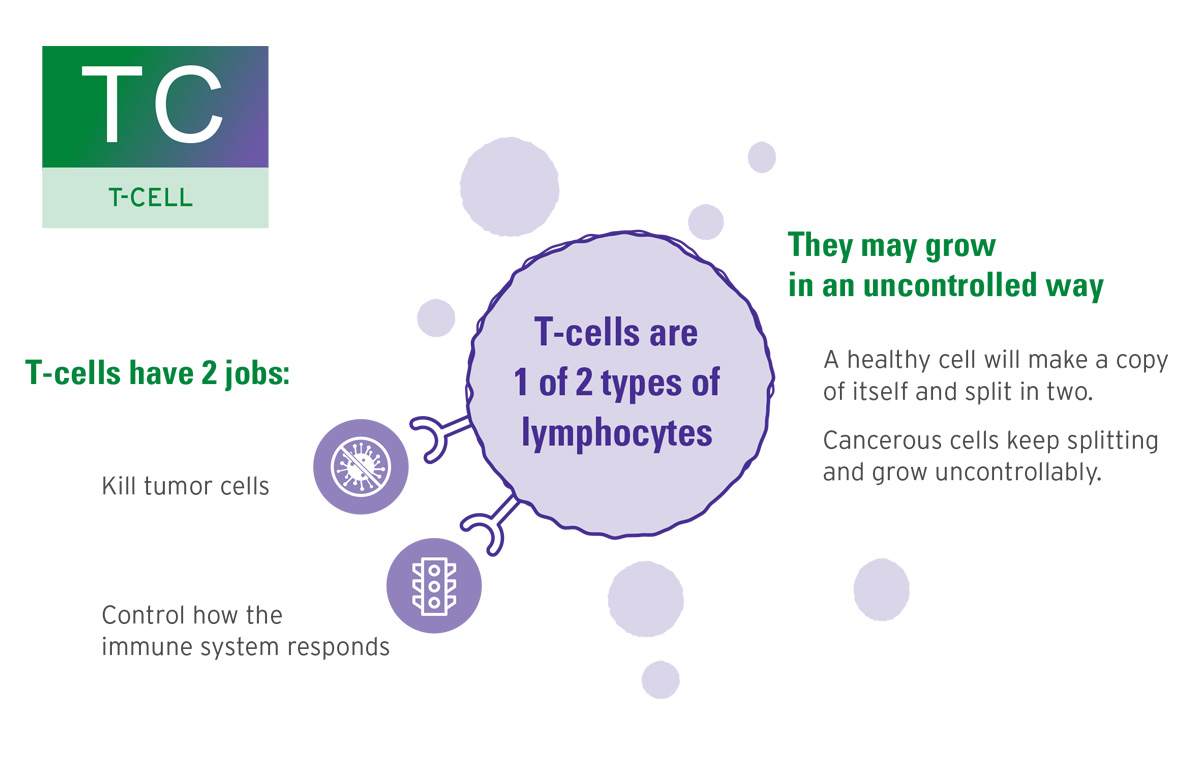
CTCL is a rare type of lymphoma. This type of cancer is caused by cancerous T-cells. T-cells are a type of white blood cell that help find and fight infection throughout the body, including in the skin. When cancerous T-cells live in the skin, it is known as Cutaneous (skin) T-cell Lymphoma.
What causes CTCL and CTCL skin symptoms?
Right now, there is no known cause of CTCL and its skin symptoms. It is not a genetic disease, so it is unlikely that you can pass it on to your children. CTCL is not contagious, so it cannot be spread to someone else.

Who is affected by CTCL and CTCL skin symptoms?
In the United States, it is thought that more than 25,000 people have CTCL. Each year, about 3,000 more people will learn they have CTCL. CTCL is hard to diagnose, so these numbers are only estimates.
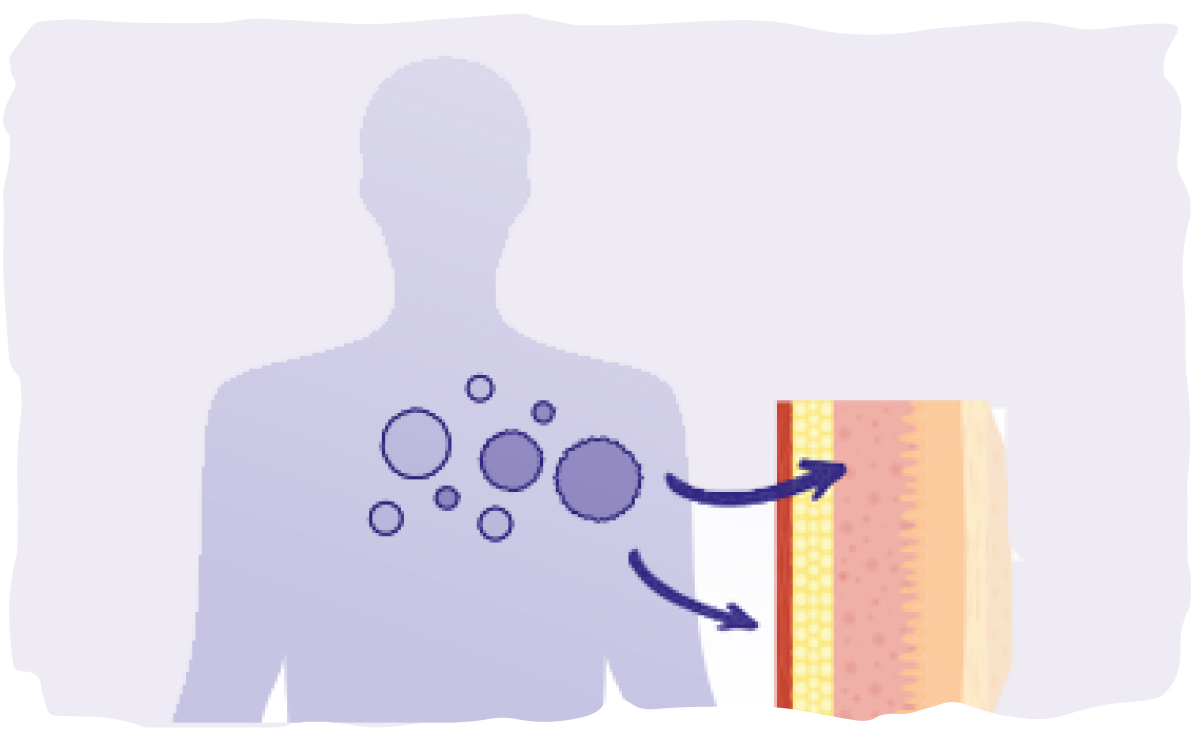
How are the symptoms I see on my skin caused by cells in my blood?
CTCL is a cancer caused when lymphocytes, a type of white blood cell, change and travel through the blood but collect in the skin.
Once there, they cause the main symptoms of CTCL.
Is CTCL skin cancer?
CTCL is a type of blood cancer, not a type of skin cancer. CTCL involves T-cells—a type of white blood cell—that change and travel through the blood and affect the skin.
Most forms of CTCL are indolent. That means that they grow slowly over time. Some types, including Sézary syndrome, can be more aggressive.
Talk with your healthcare team to be sure you know what type of CTCL you have and what treatment options can best manage your CTCL skin symptoms.
What is the difference between mycosis fungoides (MF) and Sézary syndrome (SS)?
Mycosis fungoides (MF) and Sézary syndrome (SS) are the 2 most common forms of CTCL. MF tends to progress slowly while SS can be more aggressive, with cancerous cells being found in the blood throughout the body.
The signs and symptoms of CTCL can look different in MF and SS. People with MF usually have flat, red, scaly patches, or thick, raised lesions called plaques, or large bumps. People with SS often have very itchy, scaly skin that is red all over.
Talk with your healthcare team about your signs and symptoms. Ask which type of CTCL you have, and which treatment is right for your symptoms.
How serious is CTCL?
Most forms of CTCL are indolent. That means that they grow slowly over time. Some types, including Sézary syndrome, can be more aggressive.
Talk with your healthcare team to be sure you know what type of CTCL you have and what treatment options can best manage your CTCL skin symptoms.

What are the most common CTCL skin symptoms?
Doctors have many ways of describing the skin symptoms of CTCL. For example, patches are the flat, rash-looking changes that may also make the skin scaly. Plaques are areas of skin that look like a thick, raised lesion. Bumps or nodules may also happen. Some people have one or all of these signs and symptoms. Many people also report itchy skin.
Talk with your healthcare team about your CTCL skin symptoms and what you can do to help control them.
How do the skin symptoms change in each stage of CTCL?
There are different stages of CTCL. The higher the stage, the more:
- Skin that is covered in lesions
- Severe the lesions appear
Ask your healthcare team about your CTCL skin symptoms. You may also want to download the Decision Aid to talk about what is important to you in a treatment.
Are CTCL skin symptoms contagious?
CTCL is a form of cancer caused when a certain type of blood cell changes and grows out of control. The skin symptoms are not a sign of an infection. They are not contagious and cannot be spread to another person.
Is there a cure for CTCL skin symptoms?
In rare cases, very advanced disease may be treated with a potentially curative procedure. However, it is associated with significant risks. Some treatments are able to help manage the skin symptoms of CTCL. Talk with your doctor about your CTCL skin symptoms and what you can do to help manage them.
What are the types of treatments for CTCL skin symptoms?
There are 2 main types of treatments for skin symptoms.
- Skin-directed treatments target skin
- Systemic treatments work from inside the body
Talk with your healthcare team about your CTCL skin symptoms and what treatment may be right for you.
Download our handout to learn more about CTCL skin symptoms.
Please choose "Fit to page" in your printer settings when printing this handout.
Download
Watch the video and listen to Lou’s experience with THERAKOS Photopheresis
Diagnosed with CTCL 25 years after skin symptoms first appeared, Lou was hopeful about photopheresis after trying a few other treatments but still struggling with CTCL skin symptoms.
Featured patients have been compensated for sharing their stories. Results may vary.
The health status of the patient in the video reflects his or her condition at the time the video was recorded and may have changed over time.